Nurses Frequently Delay Discharge Due To Lack Of Support For Older People
 In a new study released today, almost 70 per cent of nurses across England admit they frequently delay discharging older patients because there is no support in place for them after hospital.
In a new study released today, almost 70 per cent of nurses across England admit they frequently delay discharging older patients because there is no support in place for them after hospital.
The findings, from older people’s charity the Royal Voluntary Service, are released as A&E waiting times and delays in hospital discharge have escalated considerably, and reveal the pressures currently faced by NHS nurses in England.
The study, assisted by The King’s Fund, forms part of a campaign Let’s End Going Home Alone, which sees the charity work in partnership with communities, local authorities and NHS Trusts to provide more volunteers in hospitals and support vulnerable older people in their homes following discharge from hospital.
The value of volunteers has already been recognized by the Government, which has given £1.2m in additional grant funding for the Royal Voluntary Service, Age UK and the British Red Cross to introduce more volunteers into 29 NHS Trusts’ A&E departments but these are only a fraction of the Trusts that would benefit.
• 40% of people aged over 75 in hospital
are well enough to leave
• Family displacement and anxiety adding
pressure to hospital bed crisis
• Levying fines to relatives and patients
does not address the root cause
Almost all of the nurses surveyed (95%) reported that delayed discharge is a serious problem in the hospitals they work in and 82 per cent said it has worsened in the last 12 months.
Despite recent funding injections for some local authorities, the care crisis has reached such a level that nurses are finding that around 40 per cent of older patients are in fact medically fit for discharge, but instead are languishing in much needed beds because there is no post-hospital support in place.
Furthermore, the study found that as well as social care and in-hospital delays, families of older people anxious for them to stay in hospital for longer are also exacerbating the issue. Over half of nurses (52%) are frequently pressured by relatives to keep patients in hospital, despite them being physically well enough to leave – rising to 63 per cent on geriatric wards.
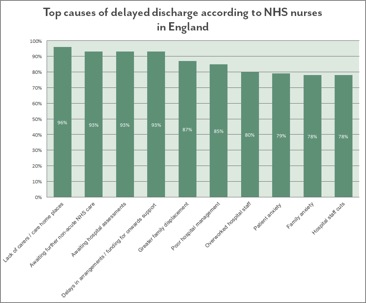 Changes in family structures and circumstances, such as divorce and relocation, raises concerns about the availability of family support for older people, and the majority of nurses (87%) say greater family displacement is having an effect on how quickly they can be discharged.
Changes in family structures and circumstances, such as divorce and relocation, raises concerns about the availability of family support for older people, and the majority of nurses (87%) say greater family displacement is having an effect on how quickly they can be discharged.
To address the problem, some NHS trusts have started to levy fines and eviction notices to patients and relatives. One in ten (10%) nurses said their hospital had issued these and more than half (58%) felt they had some effect in speeding up discharge.
However, while three quarters (75%) of nurses feel families need to take more responsibility for their older relatives, two thirds (66%) do not believe they should be blamed if there is not enough support in place. A strong majority (79%) feel levying fines does not address the heart of the issue.
Rather, nurses believe a good relationship between the NHS and social care is most important to a successful discharge policy (83%). Overall, almost three quarters (74%) believe partnering with charities and volunteers would help ease pressure on the NHS.
“This winter we have seen delays in hospital discharge reach unprecedented levels, with lack of support for older people after hospital a root cause. While additional funding has been allocated in some areas to address the crisis, many local authorities and hospital trusts are still facing budget cuts. Partnering with Home from Hospital schemes to provide greater volunteer support is a cost effective solution which helps drive important efficiencies in hospitals and enables swift, well-managed discharge from wards.
“From our experience, placing a caring volunteer at the centre of an older person’s recovery plan dramatically improves their experience, their confidence and their well-being, and helps them continue to live independent fulfilling lives. With family displacement more common, volunteers can help bridge the gap with the personal touch that relatives once filled.”
David McCullough, Chief Executive, Royal Voluntary Service
“Across the UK delayed discharges are a key indicator of the performance of not only hospitals, but how our overall health and care systems are working. In recent months, this has become a key concern for health and care systems across the country. The latest English data suggests a 23 per cent rise in the number of overall days that patients are being delayed in hospital comparing December 2014 with a year earlier.
“Volunteers can help ease some of this pressure by working with hospitals and social care to help improve transfer of elderly people to their homes. We know that those who receive these services value them highly and there are indications that this may also help reduce readmission rates too.”
David Buck, Senior Fellow, Public Health and Health Inequalities, at The King’s Fund
As part of the campaign, the Royal Voluntary Service has developed the Six Essentials it believes every older person should be entitled to experience when they leave hospital:
- Every older person should be told the plan for their return from the hospital
- Every person should be accompanied home before 10pm from hospital unless their preference is different
- Every older person needs to be able to collect their prescriptions and get to follow up appointments for a speedy recovery after a stay in hospital
- Every older person should come home from a hospital to a warm, well-lit house with someone asking how they are
- Every older person should know they’ll have help to get some shopping in and won’t have to sit hungry after a stay in a hospital
- Every older person should have a friendly face to turn to for help after a stay in hospital