Blood-Based Markers Help Spot Dementia Risk In Those With Early Memory And Thinking Problems
Researchers in Sweden found levels of certain blood-based proteins predicted worsening memory and thinking in a group of people with mild cognitive impairment (MCI).
MCI is an umbrella term given to a noticeable and measurable decline in a person’s memory or thinking, which does not interfere with activities of their daily life.
Currently the syndrome is diagnosed based on symptoms alone and it is difficult for doctors to establish an underlying cause or an accurate prognosis for any individual with MCI. While around ten to 15 percent of those living with MCI go on to develop dementia per year, a significant proportion will remain stable or improve, making this confusing and challenging for patients and doctors alike.
Researchers looked at two groups of people with MCI and measured levels of a form of tau, a hallmark Alzheimer’s protein, in people’s blood. This form of tau is known as ptau-181.
They also measured levels of another protein called, neurofilament light chain, an indicator of ongoing damage in the brain.
They found a combined measure of both of these proteins predicted a decline in memory and thinking in the volunteers over a four-year period.
The team also looked at other blood-based markers, but these did not strongly predict a change in memory and thinking.
Dr Sara Imarisio, Head of Research at Alzheimer’s Research UK, said:
“Like dementia, MCI is an umbrella term describing several symptoms, and can be caused by a number of different underlying diseases. We know that over 50% of people with MCI will go on to develop dementia, and it is important that we try to identify those who will and those who will not progress to be able to offer appropriate treatment and advice.
“Blood tests for predicting the risk of Alzheimer’s disease are getting ever more advanced. In this well-designed study, levels of a form of tau coupled with a protein indicating neurodegeneration were able to predict who developed more severe memory and thinking problems. However, further studies in larger groups of people will need to replicate and verify the accuracy of this approach.
“One intriguing finding is that these markers predicted a change in memory in thinking in both people with and without the Alzheimer’s risk gene, APOE4. Genetic testing can present ethical challenges, especially as it can have implications for a patient’s family members. A blood test that does not need a genetic test would be most beneficial in the clinic.
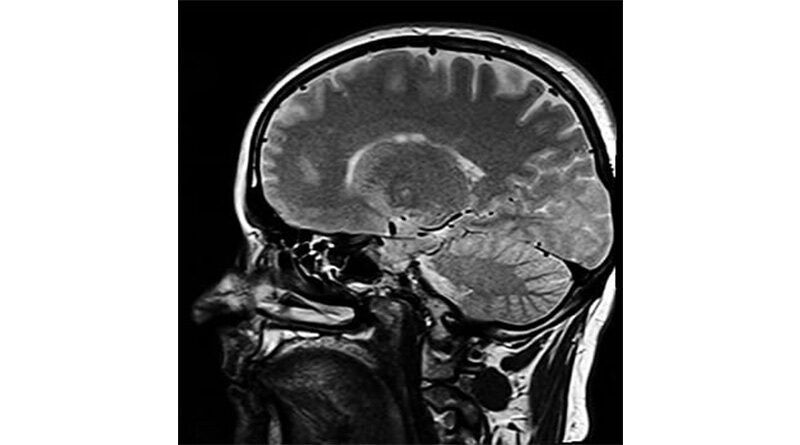
“While there are other types of biological test that can help determine the cause and likely course of memory and thinking problems, blood tests are much more affordable than brain scans and more straightforward and acceptable to people than a lumbar puncture.
“Any future dementia treatments are likely to need to be given early in the disease process, making it even more important to take findings like these forwards to improve how we diagnosis early memory and thinking problems. We need to see a shift in how we think and deal with MCI including ways to bring blood-based markers into routine clinical practice.”