Digitisation in the Adult Care Sector is Not to be Feared
By Nuno Almeida, CEO and founder of Nourish Care
The Care Quality Commission will announce new guidelines in a bid to encourage providers in the adult care sector to adhere to guidelines set out in the NHS and DHSC’s Digitising Social Care Programme. This is an extremely positive move that will improve quality, efficiency and most importantly outcomes across the sector, but some will be facing this change with trepidation and that’s understandable.
We all get used to doing things in a particular way and with change comes uncertainty. For some, even the words ‘new technology’ provoke panic. Most of us have experienced crashing apps, forgotten pin numbers and software that demands a degree in computer science and those of us in the digital care management software arena understand that first and foremost, the technology has to be user-friendly.
I see it as a pendulum and our job is to get it to swing from anxiety to empowerment. It only takes 10 minutes for a caregiver to be trained to use Nourish and we have people in their early 70s who’ve never used smartphones who are now champions of digital care.
Managers require three or four hours of training and we do that in chunks so that they can ease themselves into the platform. If you tell a care home manager that they’re going to need to take two days off to train to use a new software, they’re never going to agree to it, they just don’t have the time. We also have a helpline that is staffed by a real human being here in Bournemouth 24 hours a day. Everyone keeps talking about AI at the moment, but in my opinion, people want a real person at the end of a phone when they need help.
Once you’ve used a system like Nourish, you never want to go back. The vast majority of care workers are in the sector because they want to make a difference and for a long time, their job has been impossible. There are too many things happening all at once in their day-to-day work and staff are stretched. A care worker will be going from room to room supporting people, preparing meals etc and along the way, they must report any concerns they have about those they’re looking after.
What happens in reality is that by the time they’re interacting with the third person in their shift, they’ve forgotten what the flags for concern were with the first person they spoke to. Then, by the end of their shift when it’s time for handover, the quality of co-ordination across the team all depends on their memory and any notes they’ve managed to make during their phenomenally busy day.
This is when staff start to feel that they can’t make a difference and it takes the passion away from the job. They’re overwhelmed. In the digital world, you can record these things in real-time and instantly, everyone across the care home for example, will know that Mrs Andrew’s hydration needs to be checked. With digital record keeping, a care worker reaches the end of their shift and thinks ‘all I did was care’ because they’re not spending all their time keeping records or ending their shifts having to write laborious reports. So, we give people back a lot of time.
 We give those receiving care a voice too, in fact, that’s why I founded Nourish. For the past century really, people receiving care have been treated like a logistical problem, you know, Mrs. Andrews needs X amount of time for feeding, X for sleep and on Thursdays, she’ll do an hour of bingo, etc.
We give those receiving care a voice too, in fact, that’s why I founded Nourish. For the past century really, people receiving care have been treated like a logistical problem, you know, Mrs. Andrews needs X amount of time for feeding, X for sleep and on Thursdays, she’ll do an hour of bingo, etc.
Everybody is counting the minutes’ worth of care that Mrs. Andrews needs, but nobody is asking her or her family what she actually wants and she’s a person with likes and dislikes just like the rest of us. Perhaps she’d rather play cards than bingo.
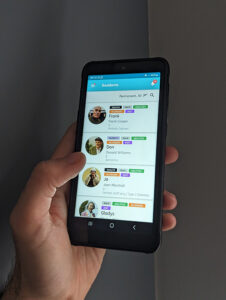
Increasingly, care workers are handing the Nourish device to those they’re caring for and giving them a choice. It’s no longer a case of, you do bingo on a Thursday and get weighed on a Tuesday morning. You’re not in a dishwasher cycle any more. Whenever there is an option for them to be asked, they can decide.
It should always be about the person, but of course, the numbers matter too, and the software takes care of those and enables the sector to deal with them as an ancillary function in the background meaning they can use every bit of their energy for caring for people.
For me, the greatest victory of digital care is keeping track of the frailty of the person receiving care over time. This means that people from the council don’t have to keep visiting to make assessments – all the information needed is there in the records. The software saves a ton of ancillary work and it gives care managers a joined-up overview of operations.
The frailty of people in care shifts over time and when that happens unnoticed, it means that the workforce is out of kilter with the people it’s supporting. 20 years ago, people were walking into care homes as a lifestyle choice because it was more sociable, a decade ago they were being wheeled in because perhaps they needed some soft dementia care, but now, very often they come in needing a high level of nursing or dementia care. We can see those trends when we look back at how things have changed over time, but with software, managers can see what they need in advance whether it be another nurse, or training in mental capacity assessments, etc. This is not something you can implement when it’s too late because then you’re operating at a high level of risk.
Being able to monitor the needs of those receiving care and helping managers respond to them instantly is where digital is going to have increasing value.
For me, one of the most rewarding aspects of Nourish is that it allows those receiving care to record how much joy they’ve experienced in a given day with a simple tap on an icon. That is the needle we should be concentrating on, the one that really matters. Whenever you care for someone, you should actively be asking how they’re feeling. The more we do that, the more we are increasing their wellbeing and that in essence, is at the very heart of caring.

